Understanding pituitary adenomas: Symptoms, diagnosis and advanced treatment
October 6, 2025
Categories: Neurology & Neurosurgery
By Anand Germanwala, MD, Neurosurgery and Chirag Patel, MD, Otolaryngology
Pituitary adenomas are among the most common brain tumors, yet they often go unnoticed until they begin to affect vision, hormone levels or overall health. These benign growths can vary widely in size, behavior and impact. For patients newly diagnosed or experiencing unexplained symptoms, understanding what a pituitary adenoma is and how it’s treated can be both empowering and reassuring.
What is a pituitary adenoma?
An adenoma is a benign (non-cancerous) tumor that originates in the tissue surrounding organs and glands. When an adenoma grows on the pituitary gland, the pea-sized endocrine gland that releases several important hormones, it’s known as a pituitary adenoma.
Around 10,000 pituitary tumors are diagnosed in the United States each year, with most of them being benign. Less than 0.1% of these adenomas will become cancerous. However, because the pituitary gland is so important for multiple bodily functions, pituitary tumors may still cause symptoms and require specialized treatment.
“They’re among the most common brain tumors. Some studies suggest up to 10% of people may have one, though many are found incidentally and never cause symptoms,” says Anand Germanwala, MD, a neurological surgeon at Loyola Medicine.
Types of pituitary adenomas
Pituitary adenomas are classified by their size and whether or not they secrete hormones.
Functional pituitary tumors
Functional pituitary tumors secrete hormones in excess which can lead to different endocrine disorders. The specific disorder will depend on the type of hormone that is being excreted.
Adrenocorticotropic hormone (ATCH)
Sometimes called corticotroph adenomas, these pituitary tumors produce ATCH which, in turn, releases too much cortisol, the stress hormone, from the adrenal glands. Eventually, this causes Cushing disease, categorized by weight gain, a rounded face, stretch marks, muscle weakness, slow healing of wounds and infections, acne, and changes in menstrual cycles and other sexual problems.
Growth hormone
These tumors are called somatotroph adenomas. Too much of the growth hormone causes acromegaly, which leads to changes in facial features, bigger hands and feet, thicker skin and joint pain.
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH)
These hormones are also known as gonadotropins. Therefore, the pituitary tumors that release an excess amount of them are called gonadotroph adenomas. However, unlike other hormones, it’s unlikely for an excess of LH and FSH to trigger symptoms. Instead, tumor pressure is more likely, causing a change in menstrual cycles, fertility problems, pain in the ovaries, enlarged testicles and elevated testosterone.
Prolactin
Excess prolactin can lead to a decrease in estrogen and testosterone, resulting in less interest in sex, breast tenderness and growth, problems with fertility and irregular or absent menstrual cycles.
“If the tumor is secreting prolactin, we can often treat it with medication that acts similarly to dopamine, which usually work very well,” says Dr. Germanwala.
Thyroid-stimulating hormone
Thyrotroph adenomas cause the thyroid gland to excrete too much of thyroxine. This leads to hyperthyroidism, speeding up the body’s metabolism leading to weight loss, rapid or irregular heartbeat, anxiety, sweating, tremors and sleep problems.
Non-functional pituitary tumors
Non-functional pituitary tumors do not produce excess hormones; instead they are often discovered incidentally while doctors are diagnosing other conditions. However, while they may not cause hormonal imbalances, they may still cause health issues depending on their size.
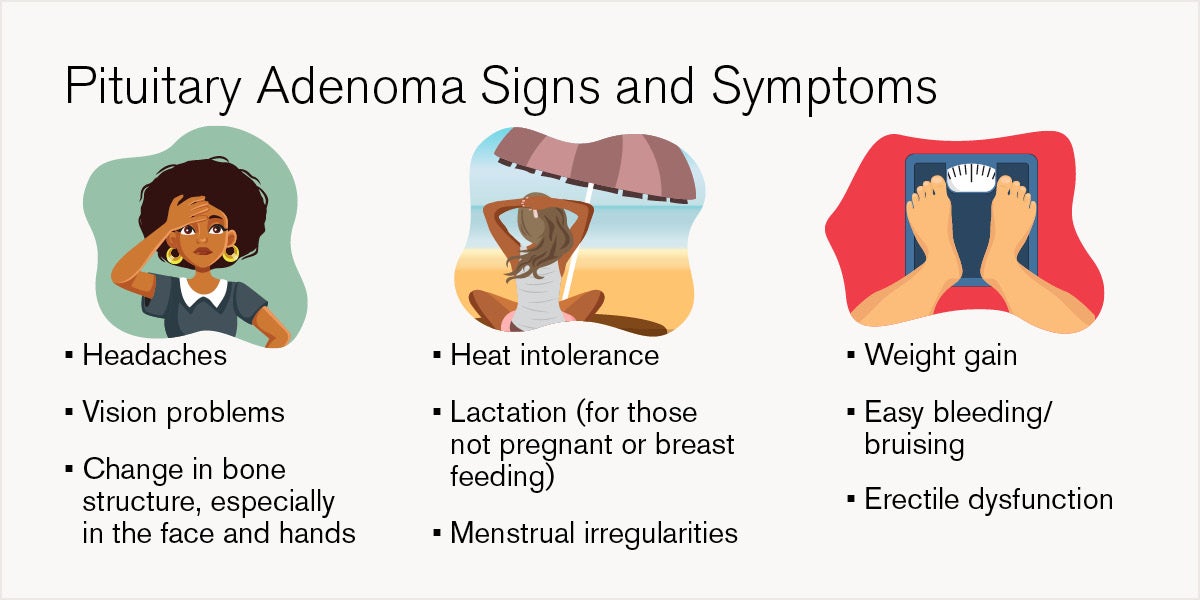
What are the symptoms of pituitary adenomas?
Not all pituitary adenomas cause symptoms. If they do, the symptoms depend on the type of excess hormones released, as is the case with functional adenomas. In the case of non-functional adenomas, they may grow large enough to press on or grow into nearby structures.
“The pituitary gland sits in a very central, high-value area of the brain. When tumors grow large enough, they can press on nearby structures, especially the optic nerves,” says Dr. Germanwala.
How are pituitary adenomas diagnosed?
In many cases, pituitary adenomas are asymptomatic and therefore not noticed or detected until a doctor is looking for a different illness or condition. It’s also possible that symptoms related to functional adenomas are similar to other medical conditions. These adenomas also tend to grow very slowly over time.
If an adenoma is detected, it’s typically because of an imaging exam, such as an MRI or CT scan, done for a different reason. Doctors order specific tests to diagnose pituitary tumors:
- Blood tests can reveal if your body is releasing too much or too little of a hormone. In some cases, a test result revealing that you’re secreting too much of a hormone is enough for a pituitary adenoma diagnosis.
- Urine tests help specifically with finding too much of ACTH.
- Vision testing. Because a pituitary tumor can affect eyesight, testing your vision is one of the simplest ways to determine if other tests are needed to detect a tumor.
How are pituitary adenomas treated?
Because pituitary adenomas are benign, many of them can simply be observed over time if they aren’t causing symptoms. However, pituitary tumors still cause serious health issues, depending on the size and if too much of a hormone is being secreted. These attributes will determine the treatment path. If treatment is needed, there are options, all with the goal of:
- Returning hormone levels to a healthy range
- Avoiding more damage to the pituitary gland and restoring its regular function
- Reversing symptoms caused by tumor pressure or preventing them from getting worse
Pituitary tumor surgical options
Sometimes, surgery is the best option if the tumor needs to be removed altogether, especially if it’s putting pressure on the optic nerves, lowering or increasing hormone levels or causing other symptoms like headaches. In general, there are two main types of surgical approaches for pituitary tumors.
Endoscopic transnasal transsphenoidal surgery (ENETS)
ENETS is the most common type of surgery to remove pituitary adenomas. A neurosurgeon, often partnering with a nose and sinus surgeon, will remove the adenoma through the nose and sinuses, avoiding any external cutting or visible scars. However, large adenomas may be difficult to remove with this surgery, especially if it has grown into other nerves or blood vessels.
Transcranial surgery
Less often used, a transcranial surgery is performed by removing the tumor through the upper part of the skull by cutting the scalp. This incision makes it easier to see and remove large tumors that have spread beyond the pituitary gland.
Radiation therapy to control adenoma growth
Often used alongside surgery, radiation therapy uses high-energy sources of radiation to control the adenoma growth, to stop the adenoma from creating excess hormones or stop the adenoma from growing back entirely after surgery.
Collaborative expertise and innovation at Loyola Medicine
The Center for Cranial Base Tumors at Loyola Medicine offers a uniquely integrated approach to treating pituitary adenomas, bringing together neurosurgery, ENT, endocrinology, ophthalmology and radiation oncology in a coordinated care model. Patients benefit from same-day consultations with fellowship-trained surgeons Dr. Anand Germanwala and Dr. Chirag Patel, streamlining the evaluation process and enhancing convenience, especially for those traveling from out of town.
“We’ve built one of the largest pituitary practices in the Chicagoland area. Patients appreciate being able to meet with the entire surgical team during a single visit, which makes the process much more convenient, especially for those traveling from out of town,” says Dr. Germanwala.
Anand Germanwala, MD, and Chirag Patel, MD, lead Loyola Medicine’s multidisciplinary approach to pituitary and skull base tumor care. Together, they bring extensive experience and nationally recognized expertise to the Center for Cranial Base Surgery.
 Dr. Germanwala is a Professor of Neurological Surgery and Residency Program Director at Loyola University Chicago Stritch School of Medicine. His clinical work is complemented by ongoing research in artificial intelligence and tumor cell modeling, helping to advance predictive tools and future therapies.
Dr. Germanwala is a Professor of Neurological Surgery and Residency Program Director at Loyola University Chicago Stritch School of Medicine. His clinical work is complemented by ongoing research in artificial intelligence and tumor cell modeling, helping to advance predictive tools and future therapies.
 Dr. Patel is a board-certified otolaryngologist and Associate Professor specializing in skull base tumors, cerebrospinal fluid leak repair, and advanced endoscopic sinus surgery. He also trained at the University of Pittsburgh, a pioneering center for skull base techniques, and plays a key role in Loyola’s collaborative surgical planning and patient care.
Dr. Patel is a board-certified otolaryngologist and Associate Professor specializing in skull base tumors, cerebrospinal fluid leak repair, and advanced endoscopic sinus surgery. He also trained at the University of Pittsburgh, a pioneering center for skull base techniques, and plays a key role in Loyola’s collaborative surgical planning and patient care.
