Diagnosing and treating benign meningioma
September 15, 2025
Categories: Neurology & Neurosurgery
Tags: Benign brain tumor, Brain tumor, meningioma
When people hear the words “brain tumor,” fear often takes over. But not all brain tumors are cancerous and advances in medicine have allowed us to control the most aggressive ones and potentially cure the more benign ones. Among benign brain tumors, meningiomas are the most common. But although benign and non-cancerous growths, they can still have a significant impact on a person’s neurological function due to their size and location.
What are meningiomas?
Meningiomas are tumors that arise from the meninges, the protective layers that surround the brain and spinal cord. While they are typically slow-growing and non-cancerous, their location within the skull means they can press on the brain or nearby nerves, leading to a variety of neurological symptoms.
“Meningiomas are the most common primary benign brain tumor that we see in adult individuals. They're almost twice as common in women as they are in men,” says Vikram Prabhu, MD, a neurological surgeon at Loyola Medicine and the Cardinal Bernardin Cancer Center.
These tumors are most common between the ages of 50 and 80 and they are more prevalent in African American populations and women. They usually occur sporadically, though in some rare instances, they may be linked to genetic conditions.
About 90% of meningiomas are classified as Grade I, meaning they are benign. The remaining 10% are Grade II or III, which are more aggressive and more likely to recur. These higher-grade tumors require more intensive treatment and monitoring.
Benign brain tumor symptoms and diagnosing meningiomas
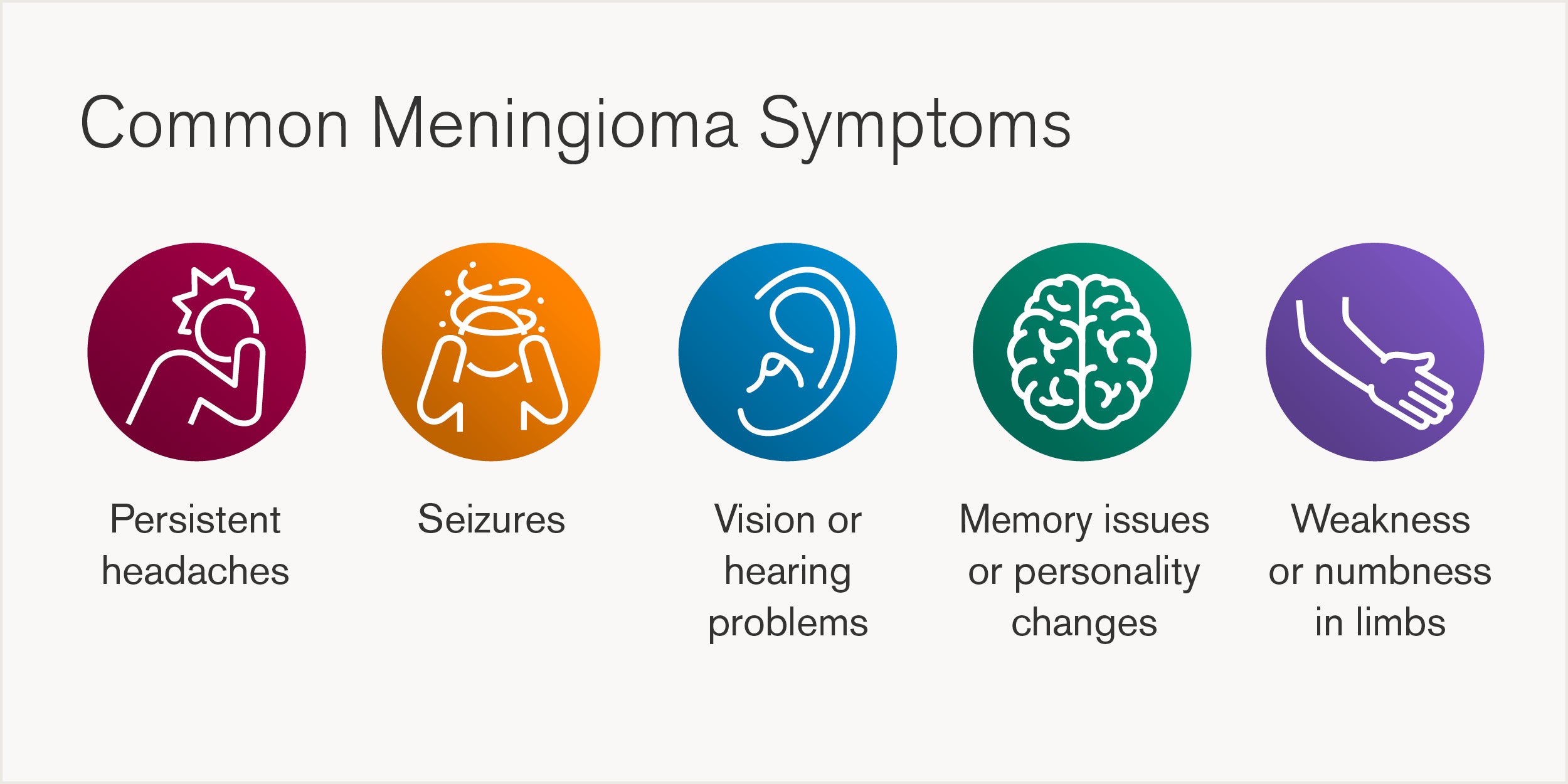
The symptoms of a meningioma depend largely on the tumor’s size and location. Some people may have no symptoms at all, while others may experience significant health challenges that greatly affect quality of life.
Because these symptoms can mimic other conditions, accurate diagnosis is critical. Many doctors use advanced imaging technologies, such as CT and MRI scans, to identify the tumor and guide treatment planning. The imaging analysis of meningiomas is also more advanced now.
“About 20 years ago, all we had was a CT scan and an MRI. Now, both have exponentially improved and we also use diagnostic angiography and embolization to eliminate arterial feeders to the tumor making surgery safer. These have revolutionized how we look at meningiomas and fortunately we have a world-class team of neuroradiologists who direct these efforts." says Dr. Prabhu.
How are meningiomas treated?
Each patient’s care is tailored based on the tumor’s size, location, growth rate, grade, and the individual’s overall health and preferences. A multidisciplinary team works together to determine the most effective and least invasive approach, always prioritizing safety, quality of life and long-term outcomes.
Observation
Observation, often referred to as “watchful waiting,” is a common approach for meningiomas that are small, asymptomatic and not growing. These tumors are frequently discovered incidentally during imaging for unrelated issues. In such cases, immediate intervention may not be necessary. Instead, patients are monitored with regular imaging and neurological evaluations to ensure the tumor remains stable.
Surgery
Surgery is the primary treatment for most meningiomas that are symptomatic, growing or exerting pressure on the brain. Surgical planning is highly individualized and supported by advanced imaging, diagnostic angiography and intraoperative tools that enhance precision and safety. While neurosurgeons lead the surgical team, other specialists such as anesthesiologists and electrophysiologists are essential to ensure a safe outcome. Specialized experienced nurses and other personnel all work together to minimize complications and promote faster recovery.
Radiation therapy
Radiation therapy becomes a key option when surgery is not feasible, either due to the tumor’s location or the patient’s overall health, or when the tumor is aggressive and has a higher risk of recurrence. Doctors may offer advanced radiation techniques, including stereotactic radiosurgery, which delivers highly focused radiation to the tumor while sparing surrounding healthy tissue.
Clinical trials and targeted therapies
Clinical trials and targeted therapies are also an important part of treatment. Some patients participate in national research studies, including a trial for Grade II meningiomas that evaluates the effectiveness of radiation versus observation after surgery. Numerous science laboratories are studying ways to treat these tumors better with medications.
Loyola’s multidisciplinary approach to meningioma care
Loyola’s strength lies in its deeply collaborative, team-based model of care. Every patient diagnosed with a meningioma is reviewed by a dedicated tumor board that meets weekly. The tumor board is led by Dr. Thakkar and Dr. Prabhu but includes other neurosurgeons, neurologists, radiologists, radiation oncologists, medical oncologists and a neuropathologist. Together, they evaluate imaging, pathology and clinical symptoms to develop a unified treatment plan.
“We meet weekly as a group to review each patient’s case both before and after surgery or to plan other treatments such as radiation therapy. We look at the patient as a whole and make decisions as a team; this ensures we have considered all options and carefully tailored the approach to the individual patient,” says Dr. Prabhu.