Resident Education
Dr. José Biller
Dr. Biller is the Chairman of the Department of Neurology and plays an integral role in the training of Loyola Neurology residents. We challenge our applicants to find another residency program in which the department chairperson is so deeply involved with day-to-day resident education and workflow. He is an author of of several widely read and comprehensive textbooks such as Practical Neurology, Localization in Clinical Neurology, Concise Neurology, The Neurologic Examination, and most recently, The Hospital Neurology Book. He has lectures and didactic sessions with the residents at least once per week and shapes much of our curriculum.
Dr. Biller is an internationally renowned academician. He has published more than 310 peer-reviewed articles, more than 130 book chapters, edited 25 books, and given more than 600 lectures around the world. He served as director of the American Board of Psychiatry and Neurology (ABPN) from 1994 to 2001 and as president of the ABPN in 2001. He is the editor of the Journal of Stroke and Cerebrovascular Diseases and Chief-Editor of Frontiers in Neurology, as well as being an editorial board member and reviewer for multiple other national and international journals and publications. The training the next generation of neurologists remains amongst his top priorities and greatest passions.
Conferences and Didactic Learning
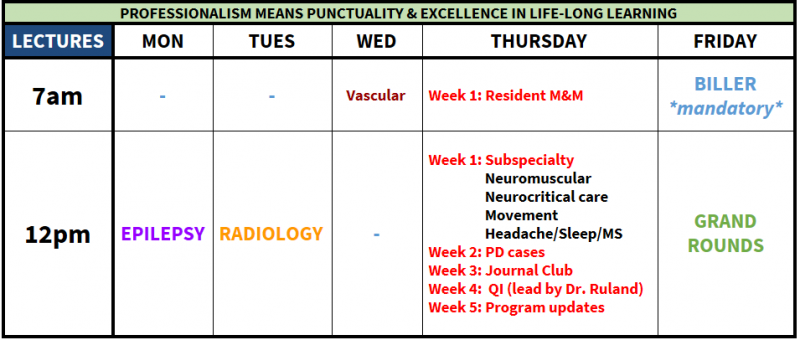
Curriculum
With the "4+2" system dividing the year into about nine blocks (six weeks per block), it seemed natural to divide the curriculum into nine major groupings and focus on one per block. Examples include: vascular neurology, neuromuscular, epilepsy, headache, etc. Within that block, Friday school sessions are dedicated to that block's subject material and there are didactic lectures by corresponding subspecialists.
Friday School
On Friday mornings, during the "+2" weeks, small groups of residents get together to present topics to each other, go over cases, and go through practice board questions. Subject material is chosen based on the current academic block the residents are in. Various afternoons are "protected time" for studying, catching up on documentation, working on their CV or fellowship applications, etc. Residents appreciate these days because they are relatively low key and a nice change of pace.
Stritch School of Medicine
We are fortunate to work closely with Loyola University Chicago's very talented and driven medical students. At Loyola, neurology is a required rotation and lasts a month. Thus, we spend large amounts of time with medical students and have the privilige of assisting in their education during their clinical years. Our residents lead formal and informal medical student lectures and also lead lumbar puncture workshops for them in the medical school's simulation center.
Neuroscience Immersion Curriculum
Every June, as our interns wrap up their PGY-1 year and transition from the Department of Medicine to the Department of Neurology, the residents and faculty work together to provide a month of orientation, lectures, simulators and guided study that we deem our "Neuroscience Immersion Month." The "Stroke Code" simulator that was developed to train our new residents has been improved upon every year, winning an AAN QI award in 2015. The "Brain Death with Family Discussion Component" simulator has expanded each year as well, recently winning an AAN QI award in 2017. A "Status Epilepticus" simulator prepares you to face this neurologic emergency with confidence, as the "Lumbar Puncture" simulator prepares you for this common bedside procedure. The month leaves plenty of time for independent study as well. We try to make sure our newbies are as prepared as possible for July 1st of PGY-2 year.
Procedural Skills
Develop skills via workshops and advanced simulation sessions – lumbar puncture, botox injection for spasticity and headache, central line placement, status epilepticus, acute stroke, brain death and breaking bad news to families.
Practice those same skills on your rotations, as well as additional opportunities to participate in cerebral catheter angiography, emergent cerebral thrombectomy, stenting, aneurysm coiling, and more.