Why robotic surgery for hernia repair may be the better option
January 28, 2026
By: Robin Favor, MD
Categories: General Surgery
Tags: hernia, hernia repair, Hernia Surgery, Robotic Assisted Surgery
Hernias are weaknesses or openings in the abdominal wall that can allow fat, or even the intestines, to bulge through. Typically, hernias are diagnosed by visual inspection and palpitation, as they often appear as lumps or bulges beneath the skin. They are a common condition often present at birth but can also be caused by injury or prior surgery, with as many as one million hernia repairs taking place every year in the United States. While not every hernia requires immediate treatment, surgical intervention is generally recommended when they cause pain, increase in size or interfere with daily activities. For patients who need surgery, a newer, minimally-invasive option, robotic hernia repair, may be the best solution.
What is robotic hernia repair?
As the name suggests, robotic hernia surgery is when a surgeon uses a robotic-assisted surgical system to help fix a hernia. The robotic instruments have joints similar to wrists and fingers that allow the doctor to be more precise and complete more complex actions that otherwise wouldn’t be possible with laparoscopic or open surgeries.
Types of hernias commonly treated
There are many types of hernias, depending on their location and what type of tissue is protruding. While robotic surgery may not be the first choice for every hernia, it can be used for the most common types, including:
- Inguinal hernias: Commonly treated robotically, benefits are clear though less dramatic compared to ventral hernias.
- Ventral hernias: Significant advantage due to ability to suture effectively on the abdominal wall.
- Hiatal hernias: Robotic approach helps navigate narrow spaces.
Robotic surgery is especially helpful for ventral hernias and abdominal wall reconstruction because the instruments can suture at angles that traditional laparoscopic tools are unable to achieve.
“Robotic surgery allows for greater flexibility. For example, one of the biggest advantages with ventral hernias is the ability to suture effectively on the abdominal wall. The wristed instruments allow surgeons to work at angles that are impossible with traditional straight instruments, making the repair more precise and efficient,” says Dr. Favor, general surgeon at MacNeal Hospital.
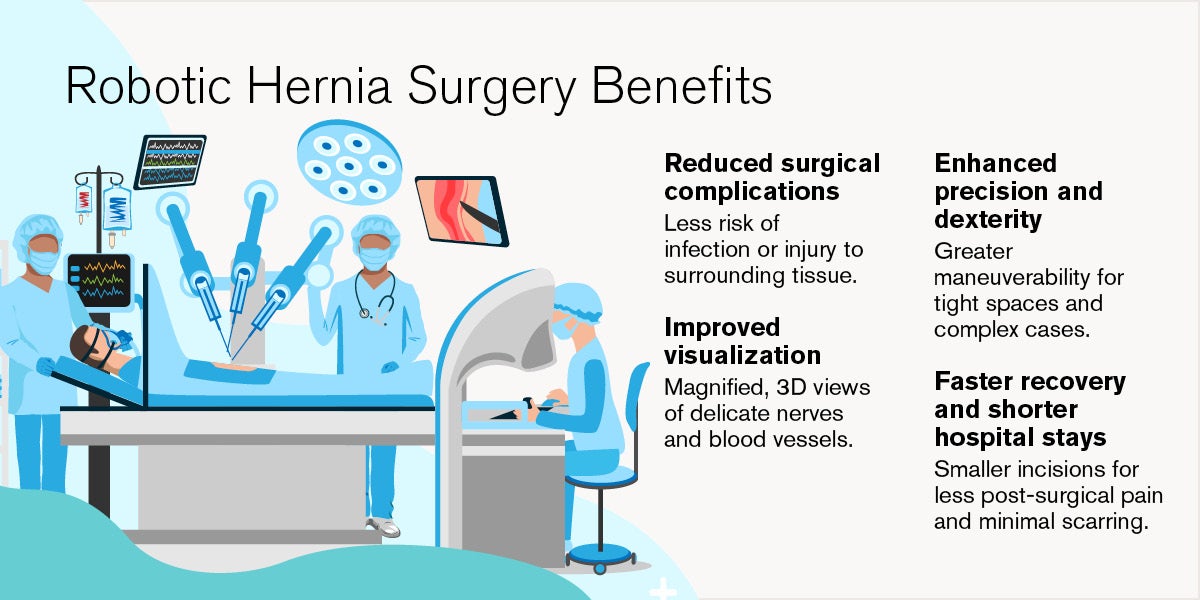
What are the benefits of robotic hernia surgery?
Patients who undergo robotic hernia surgery typically experience a much more comfortable recovery compared to traditional approaches. Postoperative pain is significantly reduced, which means they can return to their normal activities and work much sooner. Hospital stays are also shorter; ventral hernia patients who might spend one or two nights in the hospital after a laparoscopic procedure usually go home the same day with a robotic repair. Inguinal hernia patients also benefit from less pain, even though both approaches generally allow same-day discharge. In general, robotic surgery offers faster recovery, less discomfort and generally lower complication rates.
“In most cases, I choose the robotic approach because it allows for a better operation overall. The technology offers improved instrumentation and visualization, which translates to better outcomes,” says Dr. Favor.
Who qualifies for robotic hernia surgery?
While many surgeons prefer the robotic approach due to improved visualization and better handling, robotic surgery is not a one-size-fits-all solution, and not every patient is a candidate. A patient’s overall health, the complexity of the repair and a patient’s previous surgeries all determine their candidacy.
Some patients also may not qualify due to factors such as extremely large hernias, extensive scar tissue from previous abdominal surgeries or other complications, such as a large tumor. In these situations, a different approach, such as open or laparoscopic surgery, may be safer and more effective. Ultimately, the decision is made on a case-by-case basis, with the surgeon considering the patient’s unique anatomy and medical history.
“Robotic surgery significantly reduces the need to convert to an open procedure. Without robotic tools, surgeons would have to open more cases, especially in patients with higher BMI or complex anatomy,” says Dr. Favor.
Robotic hernia repair at Loyola Medicine
At Loyola Medicine, patients benefit from a team of highly experienced, fellowship‑trained surgeons who are leaders in minimally invasive and robotic techniques. Our surgeons perform a high volume of robotic hernia repairs each year, bringing advanced skill, precision and clinical judgment to every procedure. This depth of experience helps ensure safer operations, smoother recoveries and long‑term strength of repair.
Loyola Medicine is also home to some of the most advanced surgical technology available today, including state‑of‑the‑art robotic platforms that offer enhanced visualization, improved dexterity and unmatched accuracy in complex spaces. These tools allow our surgeons to tailor each repair to the patient’s unique anatomy, an approach that supports better outcomes and reduces the need for conversions to open surgery.

