Why metabolic (bariatric) surgery is still the most effective solution for weight loss
December 18, 2025
By: Tyler Cohn, MD
Categories: Bariatric and Metabolic Surgery, Bariatric Surgery, Bariatrics
Tags: weight loss, Bariatric Surgery, Bariatrics
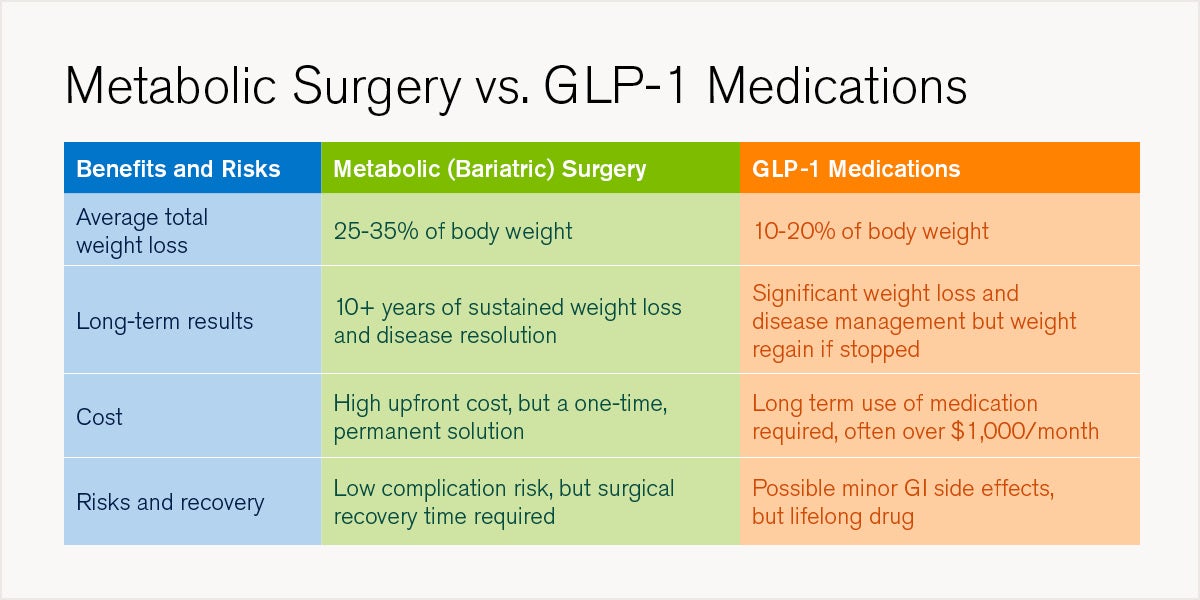
The use of glucagon-like peptide-1 (GLP-1) agonists for weight loss has exploded in the last few years. Since 2020, the number of prescriptions made for these drugs has tripled, and it’s estimated that 12% of Americans have used these medications. They are transforming the landscape of weight loss and making both patients and physicians re-evaluate traditional approaches. However, while these drugs have a place in the fight against obesity, metabolic (bariatric) surgery remains the most effective, long-term solution for severe obesity and metabolic diseases.
“Newer medications, including GLP-1 drugs, can help patients successfully lose weight to a lesser degree than bariatric surgery. Unfortunately, if these medications are stopped, patients regain almost 70% of their lost weight on average within one year. The only treatment that has consistently demonstrated long-term success in managing obesity is metabolic surgery,” says Tyler Cohn, MD, interim director, division of minimally invasive, bariatric and community general surgery at Loyola Medicine.
What is metabolic surgery?
Metabolism is the process by which our bodies use enzymes – proteins that help speed up chemical reactions in our bodies – to break down food and other biological substances to then produce energy needed for daily living.
Metabolic surgery, also referred to as bariatric surgery, has a profound effect on metabolism that greatly accelerates weight loss. In general, these surgeries modify the stomach and intestines to treat obesity and related diseases by making the stomach smaller and/or bypassing a portion of the intestine. This leads to complex changes in hormones that control metabolism resulting in less food intake, decreased hunger, increased fullness and, ultimately, changes how the body absorbs food for energy.
“Metabolic surgery triggers a complex cascade of hormonal and metabolic changes that influence hunger, satiety and fat metabolism. Unlike GLP-1 medications that target one or two pathways, surgery resets multiple signaling systems, creating a more comprehensive and permanent effect on weight regulation,” says Dr. Cohn.
Not all metabolic surgeries are the same. There are many different types, each with their own advantages and drawbacks. Your bariatric surgeon will look at your health history and discuss your goals for your health and weight loss to help determine which one is right for you. The most common procedures are:
- Roux-en-Y gastric bypass: The top portion of the stomach is shrunk and separated from the remainder of the stomach then attached to the middle of the small intestine. A second connection is created in the small intestine to redirect the flow of digestive juices.
- Sleeve gastrectomy: The stomach is divided vertically with a special tool, removing 70 to 80% from the body. Its shape now looks like a tube, banana or “sleeve” that restricts the amount of food consumption.
- Duodenal switch: This combines a sleeve gastrectomy (described above) with an intestinal bypass, resulting in the benefits of both the sleeve and Roux-en-Y.
- Gastric banding: An adjustable silicone band filled with saline is wrapped around a part of the stomach, creating a small pouch that restricts the intake of food. This procedure is rarely ever performed due to risks of long-term complications
The benefits of metabolic and bariatric surgery
Despite the growing prescriptions for GLP-1 medications, metabolic surgery continues to be the most effective and long-lasting treatment for obesity, as well as for the remission of cardiovascular diseases, diabetes and even certain cancers. Statistics on effectiveness of these procedures include:
- Reduces the risk of premature death by up to 50%
- Patients may lose as much as 60% of excess weight six months after surgery and over 75% a year after surgery
- Many patients experience remission or resolution of obesity-related diseases
- The vast majority of patients maintain their weight loss 10+ years after surgery
These metabolic procedures are also incredibly safe. They are considered to have less risk than some of the most performed surgeries in the United States, such as gallbladder surgery and even knee replacement.
The drawbacks of GLP-1 medications
It may seem like everyone is taking GLP-1 agonists. Their original use was for the management of blood sugar levels for people with Type 2 diabetes. Weight loss was an observed side effect during early trials for these medications.
Now, from celebrities to people you may personally know, the increase in prescriptions for these medications can’t be understated. Over the last few years, there has been a 700% increase in the number of patients without diabetes starting treatment regiments of GLP-1 medications. However, there are many drawbacks that commercials and marketing campaigns don’t tell you.
Weight regain and unrealistic expectations
These medications are not a permanent solution. The average person regains 68% of their weight within one year of stopping GLP-1 medications. And 85% gain back at least half of their weight within one year.
To maintain results, patients must stay on GLP-1s indefinitely. They are often not told this upfront and, with many people stopping these drugs after only two years due to this misunderstanding, high costs, and side effects, it can lead to them possibly giving up on weight loss all together.
“In my experience, most patients are not informed that GLP-1 medications require ongoing use to maintain results. This lack of upfront education often leads to unrealistic expectations and disappointment when weight returns after discontinuation,” says Dr. Cohn.
Side effects and unknown long-term outcomes
Because of the relative newness of GLP-1 medications, long-term effects beyond a few years of use are unknown. There is also uncertainty whether or not weight loss will remain even with continued usage of the medication after five years. Side effects can also occur, such as:
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Gastroparesis (delayed stomach emptying)
- Pancreatitis
- Possible increased risk of sudden blindness
Cost and insurance coverage
Health insurance coverage varies widely for GLP-1 medications and can cost a patient hundreds of dollars per month. Even with insurance, rising premiums may make these agonists unaffordable for many people. And because these medications need to be taken consistently over many years, the costs incurred may surpass that of metabolic surgery after less than a year. It can also be easier for insurance companies to cover bariatric surgery due to it being a one-time, permanent solution for weight loss, rather than an ongoing medication.
How metabolic surgery and GLP-1 medications can work together
Despite the drawbacks of GLP-1 agonists, they can still be a powerful tool for weight loss when used together with metabolic surgery at the discretion of your physician. Both surgery and GLP-1s are part of a continuum of treatments for obesity. There is no single cure, and both approaches can play a role in helping patients manage their weight.
Many patients begin their journey with medications and later move on to surgery when they need more permanent results. Likewise, some patients who have had surgery may use GLP-1 drugs afterward to lose additional weight or address weight regain. These treatments can complement each other, offering flexibility based on individual needs and goals.
“We now view GLP-1 medications and metabolic surgery as complementary treatments rather than competing options. Each plays a role, allowing for personalized strategies that address the complexity of obesity,” says Dr. Cohn.
Metabolic surgery and weight loss at Loyola Medicine
At Loyola Medicine, our nationally recognized Center for Metabolic Surgery & Bariatric Care offers both medical and surgical options to help patients achieve and maintain a healthy weight. Designated as a Comprehensive Center by the American College of Surgeons, Loyola provides expert care backed by the resources of a leading academic medical institution.
Our multidisciplinary team includes bariatric surgeons, medical weight loss physicians, advanced practice nurses, registered dietitians and health psychologists. Together, they create individualized plans that address the medical, nutritional and behavioral aspects of weight management. Whether you choose a non-surgical program or a surgical procedure, you’ll receive comprehensive support before, during and after treatment.