Trigeminal neuralgia explained: Symptoms, causes and treatment options
December 18, 2025
Categories: Neurology & Neurosurgery
Tags: Neurological Surgery, Trigeminal neuralgia, facial pain, Cranial nerve, facial nerve disease
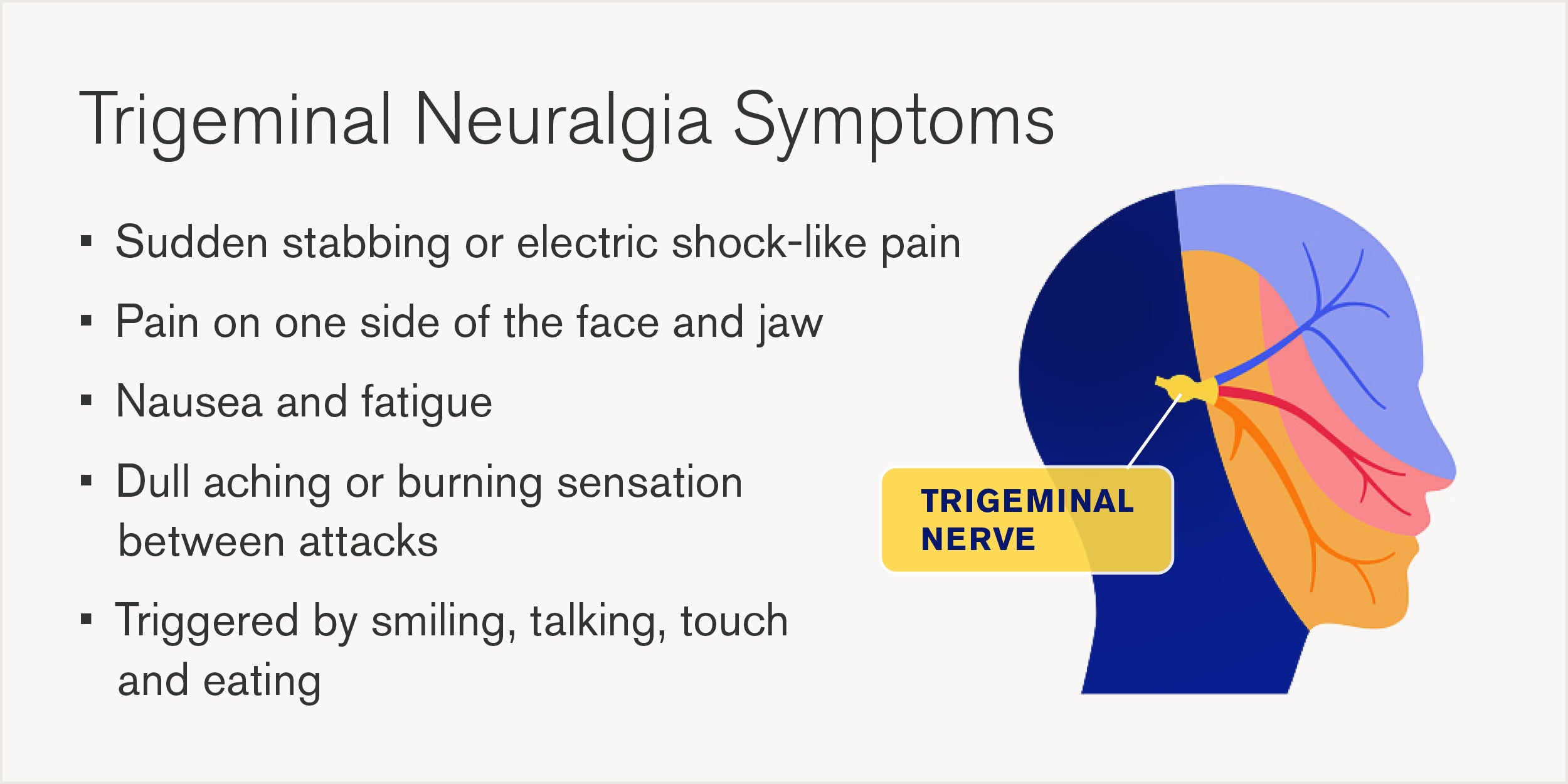
Trigeminal neuralgia is a chronic neurological condition that primarily affects the trigeminal nerve, causing intense, stabbing and electric shock-like pain in any trigeminal nerve distribution. This extreme pain can be triggered by everyday activities like brushing your teeth, smiling or even a gust of wind, making it physically and mentally debilitating for anyone living with the condition. While there is no cure for trigeminal neuralgia, several treatment options are available to help manage and often eliminate the pain.
“Unfortunately, trigeminal neuralgia is often described as one of the most severe forms of facial pain, making even routine activities like eating or speaking extremely challenging,” says Brandon Zsigray, MD, neurosurgeon at Loyola Medicine.
What is the trigeminal nerve?
Trigeminal neuralgia is caused by irritation of the trigeminal nerves, one set of cranial nerves in the head which branches out to the forehead, cheek and lower jaw. These nerves are responsible for providing sensation to the face. One trigeminal nerve runs to the right side of the head while another goes to the left, each with three branches. These three branches are the:
- Ophthalmic nerve, which controls sensation in the eye, upper eyelid and forehead.
- Maxillary nerve, which controls sensation in the lower eyelid, cheek, nostril, upper lip and gum.
- Mandibular nerve, which controls sensation in the jaw, lower lip and gum, and some of the chewing muscles.
What causes trigeminal neuralgia?
It’s estimated that 1 in 15,000 people currently suffer from trigeminal neuralgia, although this number may be higher due to misdiagnosis of pain symptoms. The exact cause of the condition is still not understood, but doctors have a good idea depending on the type of trigeminal neuralgia, which can be primary or secondary.
- Primary trigeminal neuralgia is likely caused by an artery or vein compressing one or more branches of the trigeminal nerve, causing it to misfire.
- Secondary trigeminal neuralgia is caused by a similar pressure but from a tumor, cyst, facial injury, or another medical condition that damages the myelin sheaths, the protective membrane around nerve cells that provides insulation and helps with fast electrical impulses.
Trigeminal neuralgia usually appears suddenly, without warning. However, some patients say the pain started after an accident, injury or dental work. Because the symptoms – sharp, burning, throbbing or shock-like pain around the face – can be caused by many different conditions, including other pain disorders, diagnosis can be difficult, relying primarily on symptoms and medical history. Doctors base their diagnosis on the location, triggers and type of pain.
“When this nerve becomes irritated or compressed, the resulting pain can be disproportionate to the trigger, which is why the condition feels so unpredictable,” says Dr. Zsigray.
Medical treatment for trigeminal neuralgia
When trigeminal neuralgia is diagnosed, the first-line, gold standard of medical therapy is carbamazepine, an anti-epileptic medication. It works by reducing abnormal nerve impulses caused by nerve irritation and myelin sheath breakdown. Other medications for neuropathic pain, such as gabapentin, may also be used. None of these drugs cure the condition, instead managing the symptoms slowing down nerve misfiring.
The primary side effects are dizziness and electrolyte imbalance. However, if the drug is well-tolerated and provides relief then patients usually stay on the medication their entire life.
“Medical treatment focuses on symptom control rather than reversing nerve damage, which is why consistent monitoring and dose adjustments are essential,” says Dr. Zsigray.
Microvascular decompression for facial nerve pain relief
If medication does not provide enough facial nerve pain relief, or the side effects are not well-tolerated by the patient, then surgery can be considered. One common surgical option is microvascular decompression. During this procedure, the blood vessel is dissected away from the nerve and padding is placed between them. While this method often proves highly effective and patients report complete or substantial pain relief, there is a risk of symptoms reoccurring over time.
“For many patients, surgical intervention significantly improves quality of life, allowing them to resume normal activities with reduced pain,” says Dr. Zsigray.
Comprehensive neurological care at Loyola Medicine
Loyola Medicine offers one of the most comprehensive and advanced neurosurgery departments in the nation, providing a multidisciplinary approach to care and dedicated support services for patients and families. As an academic medical center, Loyola delivers compassionate, exceptional care to patients and trains future leaders in neurology and neurosurgery.
Loyola’s expert neurosurgeons are highly skilled in the surgical treatment of a wide range of neurologic conditions, including the treatment of trigeminal neuralgia. Through collaboration with subspecialists such as neurologists, otolaryngologists, pediatric surgeons and radiation oncologists, the Loyola health care team provides individualized treatment plans to address specific conditions using the most advanced techniques and technology available.

