How low-dose radiation therapy helps with plantar fasciitis pain
September 25, 2025
Categories: Orthopaedics
Tags: plantar fasciitis, intensity modulated radiation therapy, Low-dose radiation therapy, LDRT
By Matthew Harkenrider, MD and Marissa Mullins, APRN, Department of Radiation Oncology
Millions of Americans live with chronic musculoskeletal pain, which can originate from muscles, joints, tendons, or connective tissues in the body. Plantar fasciitis is an inflammatory condition of the thick band of tissue that connects the heel bone to the toes. Foot and heel pain from plantar fasciitis is a very challenging disorder to treat, especially for those who are active or spend long hours on their feet.
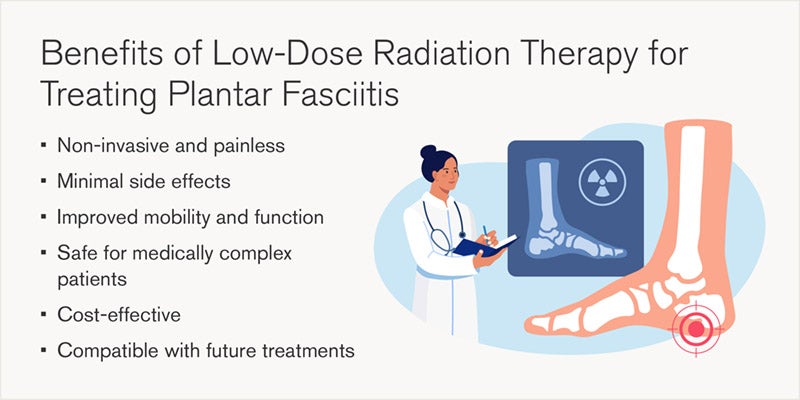
While some patients with plantar fasciitis improve with rest, stretching, orthotics and/or physical therapy, some patients experience persistent pain despite conventional treatment. For these individuals, low-dose radiation therapy (LDRT) offers a safe, effective and non-invasive alternative for pain relief.
“We’ve seen patients go from barely moving to walking their dog again,” says Marissa Mullins, APRN, a nurse practitioner specializing in radiation medicine at Loyola Medicine. “It’s not just about pain relief. It’s about restoring quality of life.”
Understanding low-dose radiation therapy for chronic heel pain
Low-dose radiation therapy is a targeted form of x-ray treatment. This particular therapy uses a fraction of the dose used in cancer care. LDRT works by altering the immune response of the affected area by calming the inflammatory cells that contribute to pain and stiffness. In the case of refractory plantar fasciitis not responsive to conservative therapies, low dose radiation therapy may be an alternative option to treat the affected part of the foot and heel.
Radiation therapy has been safely used for over a century to treat painful inflammatory conditions, including plantar fasciitis.
“Radiation in low doses acts as an immunomodulator,” explains Dr. Harkenrider. “It turns down the dial on pain by calming the cells that create the inflammatory response in the affected tendons and joints.”
How low-dose radiation therapy works for plantar fasciitis
Pain from plantar fasciitis often stems from inflammatory cytokines, proteins that signal the body to respond to injury or stress. When this pain is chronic, these signals persist, causing ongoing discomfort. LDRT reduces the production of these cytokines, interrupting the pain cascade and allowing tissues to heal. Unlike traditional medications, LDRT targets the source of inflammation directly. The result is reduced pain, improved mobility, and enhanced quality of life.
Why choose low-dose radiation therapy for heel pain relief?
For patients living with persistent foot and heel pain from plantar fasciitis, low-dose radiation therapy can be an effective alternative, especially when conservative treatments have failed. It is also particularly beneficial for individuals with conditions like osteoarthritis, tendonitis, or bursitis who are seeking safe, effective relief without the risks of more aggressive interventions.
Who is a good candidate for LDRT?
Low-dose radiation therapy is typically recommended for patients:
- Over the age of 40
- Experiencing chronic pain for 6+ months
- Who have not responded to conservative treatments
- Who are not candidates for surgery due to age or medical conditions
Imaging may be used to confirm diagnosis, but the most important factor is a documented history of persistent pain from plantar fasciitis. Low dose radiation therapy does not prevent future surgery and can be used as a bridge between other treatments.
What to expect during low-dose radiation therapy for plantar fasciitis
Patients with painful plantar fasciitis begin with a thorough evaluation by a radiation medicine provider. Medical history, prior treatments and imaging are reviewed to determine eligibility. Insurance and Medicare routinely covers this treatment, so once approved, patients undergo a planning session to map the plantar fascia. A custom mold is used to support the leg and foot during therapy.
Patients receive six sessions over two weeks, with each treatment taking about 30 minutes door to door. The therapy is painless, and patients can drive themselves to and from appointments. Two months after treatment, patients return for a follow-up to assess pain relief and functionality. If needed, a second course may be considered.
Fill out the form online to request an appointment with a Loyola Medicine specialist for osteoarthritis treatment.