Uterine fibroids: Symptoms, treatments and when to seek care
January 6, 2026
Uterine fibroids are one of the most common health concerns for women, yet they’re often misunderstood. These noncancerous growths can range from tiny nodules to large masses that change the shape of the uterus. While many women never experience symptoms, others face significant discomfort and complications. Learning more about fibroids and your treatment options can help you make informed decisions about your care.
What are uterine fibroids?
Uterine fibroids are benign tumors of muscle tissue in, on and around the uterus. They can vary in size and may enlarge or distort the uterus and in some cases, the cervix. While the exact cause of uterine fibroids is not fully understood, both genetics and hormones play key roles.
Fibroids are more common in African American women, and having a family history may increase likelihood for developing them. Hormones like estrogen and progesterone may trigger fibroid growth, which helps explain why new fibroids rarely form after menopause and existing ones shrink when hormone levels drop. The latest research also suggests that nutrition and lifestyle choices have little to no effect on the growth and development of uterine fibroids.
“I describe uterine fibroids as a benign muscle growth of the uterus to patients, and they can really range in size from very small—kind of like skin tags of the uterus—to very large, causing symptoms,” says Laura Glaser, MD, obstetrician and gynecologist at Loyola Medicine.
Uterine fibroids affect the majority of women
Uterine fibroids are incredibly common. By the time menopause occurs, 80% of African American women and 70% of Caucasian women will have had them. Overall, half of the women in the world have at least one fibroid before menopause. Despite the high occurrence, however, most do not require treatment.
Uterine fibroid symptoms and health implications
Fibroids usually become apparent during reproductive years. However, many women will not experience symptoms or require treatment for them. The size and location of the fibroids will determine the symptoms and treatment strategy, if necessary.
Almost all fibroids are found inside the uterus, in the uterine wall, and/or on the outside of the uterus. These fibroids are divided into three categories depending on their location:
- Subserosal are on the outer wall of the uterus.
- Intramural are in the muscle layers of the uterine wall.
- Submucosal protrude into the uterine cavity.
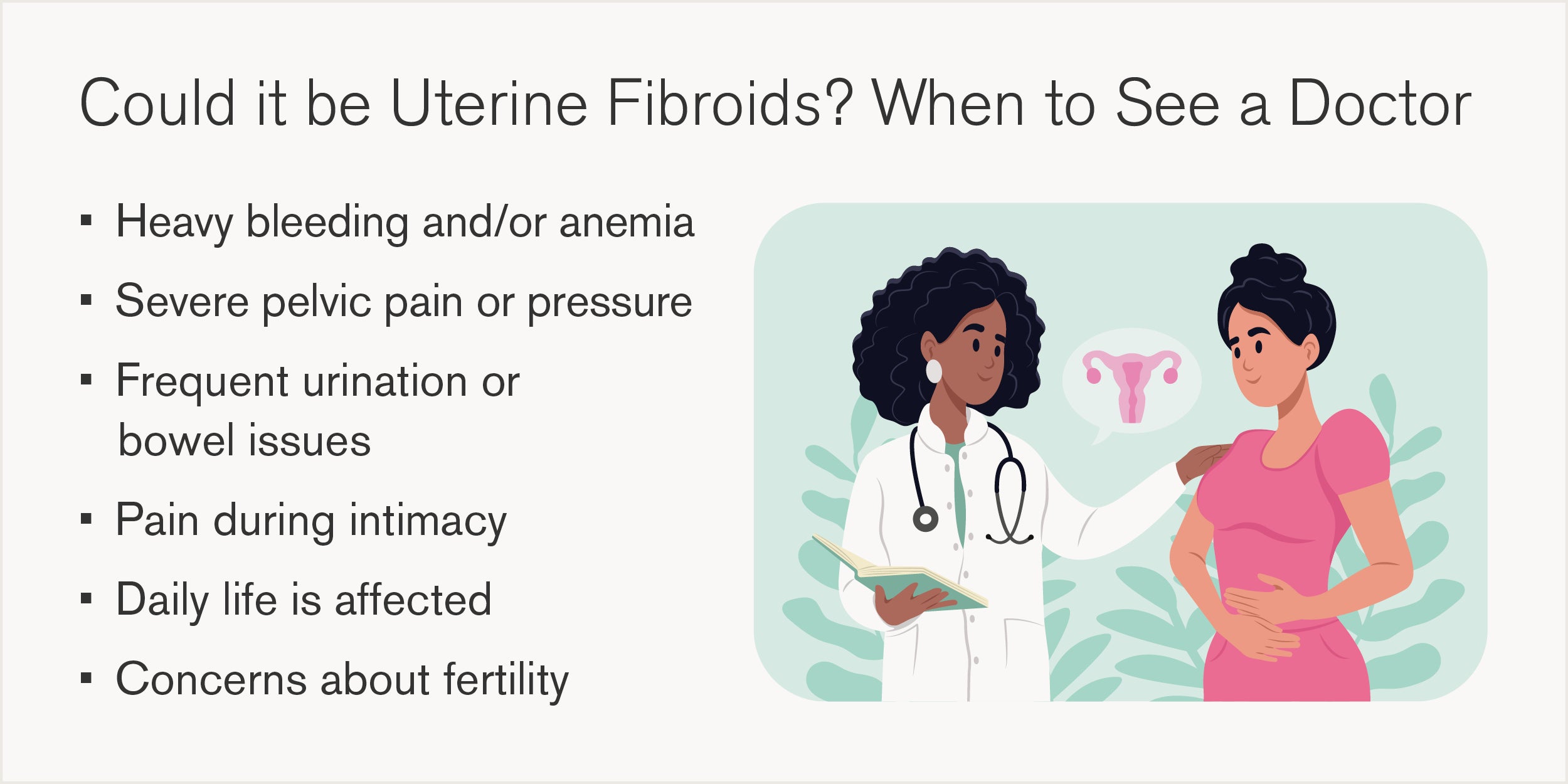
Most women with fibroids have no symptoms. When symptoms do occur, the most common are abnormal uterine bleeding, pain and pelvic pressure. Less common symptoms include infertility, heavy or painful periods, frequent urination and constipation.
“Size and location make a big difference. Fibroids inside the inner cavity of the uterus tend to cause heavier bleeding, while those on the outside often cause pain, pressure and bowel or bladder symptoms,” says Dr. Glaser.
Can uterine fibroids affect fertility and pregnancy?
Generally, many women with fibroids can become pregnant and have healthy pregnancies. However, it’s important to speak with a gynecologist about your specific needs. Compared to those without fibroids or those who have had them removed, women with fibroids may find it more challenging to become pregnant. The success rates of in vitro fertilization can also be lower when fibroids are present.
The location of the fibroids also matters. If they are protruding into the uterine cavity or are inside of the muscular layer, the position of the baby can change at the time of delivery or cause other problems. Women with fibroids have an increased risk for a caesarean section, miscarriage or premature delivery.
How are uterine fibroids diagnosed?
If a doctor needs to check for uterine fibroids, there are four options they typically use. They include:
- Pelvic exams: By checking the size and shape of the uterus, doctors can find many uterine fibroids and determine if they have grown.
- Ultrasound: Using echoes from high-frequency sound waves, a picture is formed of the pelvic organs.
- Sonohysterography: A type of ultrasound that sends a small amount of fluid into the uterine cavity to help determine if fibroids are distorting or protruding.
- Magnetic resonance imaging: An MRI uses magnetic fields to generate detailed images of the uterus to help determine the size and location of fibroids.
Treatment options and recovery
Treatment for uterine fibroids is highly individualized. Your doctor will consider factors such as symptom severity, fibroid size and location, age and whether you want to preserve fertility. It’s important to know that fibroids can return after non-surgical treatments, so regular follow-up helps monitor regrowth.
“Fibroids can reoccur. Unfortunately, the vast majority do. It’s in the range of 75%, though not always to the degree that they cause major issues,” says Dr. Glaser.
Non-surgical treatments
Certain medications like hormonal birth control or GnRH agonists can help manage heavy bleeding and shrink fibroids temporarily. These are often used for symptom control or as a bridge for surgery. For women with anemia caused by bleeding from the fibroids, iron supplements can help.
Minimally-invasive procedures
- Uterine artery embolization: A radiologist injects tiny particles into the uterine arteries to block blood flow to fibroids, causing them to shrink. Recovery is typically one to two weeks.
- MRI-guided focused ultrasound: Uses high-frequency sound waves to destroy fibroid tissue without incisions.
- Laparoscopic or robotic myomectomy: Removes fibroids through small incisions while preserving the uterus. Recovery is usually two to four weeks.
Surgical options
- Myomectomy: Removes fibroids but keeps the uterus intact. This option is ideal for women planning pregnancy and can be performed abdominally (through the abdomen), laparoscopically (small incisions), or hysteroscopically (through the cervix).
- Hysterectomy: Removes the uterus entirely, eliminating fibroids permanently. This option is considered only when fibroids are extremely large, the patient has uncontrollable bleeding or is suffering from other symptoms that are affecting daily life.
Advanced treatments for gynecologic conditions at Loyola Medicine
At Loyola Medicine, we combine advanced technology with a patient-first approach. Our gynecological specialists offer comprehensive care, from accurate diagnosis to minimally-invasive procedures and complex surgeries. We work closely with each patient to create a personalized treatment plan that prioritizes comfort, safety and long-term health.
“Patients have many options for treatment. It doesn’t have to be medications or invasive surgery. There are methods that use electromagnetic energy and focused ultrasound to zap fibroids without a big surgery. These will likely become more common in the future,” says Dr. Glaser.

