Understanding Microscopic Colitis: What to Know About This Overlooked Digestive Condition
June 13, 2025
Categories: Digestive Health
Tags: Colitis, Microcolitis, Microscopic colitis
By Dejan Micic, MD, Digestive Health
Microscopic colitis is a lesser-known but common cause of chronic diarrhea. Many people may not realize they have it, especially since symptoms can look like other digestive problems. It affects mostly older adults, especially women, and can greatly impact daily life.
While it’s not as widely talked about as Crohn’s disease or ulcerative colitis, it deserves attention, especially if you’re living with frequent, watery bowel movements and don’t know why. Loyola Medicine is here to help you understand this condition, from symptoms to treatment.
What is microscopic colitis?
Microscopic colitis is a form of inflammatory bowel disease (IBD), but unlike Crohn’s disease or ulcerative colitis, it’s not visible during a standard colonoscopy. The inflammation is only seen under a microscope when small tissue samples (biopsies) from the colon are examined. That’s how the condition got its name.
There are two main types:
- Collagenous colitis: This form features a thickened layer of collagen (a protein) just beneath the lining of the colon.
- Lymphocytic colitis: This type shows an increased number of lymphocytes (a type of white blood cell) in the colon lining.
Microscopic colitis is most common in adults between the ages of 50 and 70 and it affects women more than men. Some studies suggest it may be underdiagnosed, emphasizing the need for those with symptoms to see a physician.
“Microscopic colitis is a very common cause of diarrhea that really impacts a different subset of the population compared to inflammatory bowel disease,” says Dejan Micic, MD, a gastroenterologist at Loyola Medicine. “The colonoscopy itself can look normal. But as the name states, there’s inflammation on the biopsies that we take.”
Common symptoms of microscopic colitis
The key symptom is watery, non-bloody diarrhea that lasts for weeks or months. Many people will experience diarrhea first thing in the morning or shortly after eating. Some patients may have four to six bowel movements in a short span of time.
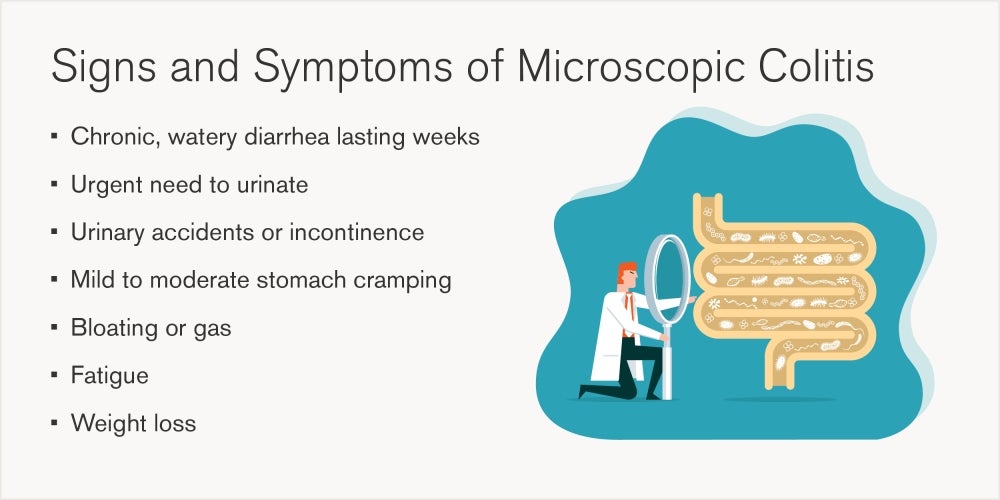
Over time, patients may start avoiding food to prevent symptoms, which can lead to nutritional deficiencies, especially vitamins D and B-12. Because the symptoms overlap with other GI issues, microscopic colitis often goes undiagnosed without a biopsy.
“Any diarrhea that’s persisting for more than two weeks requires some degree of evaluation,” says Dr. Micic.
Microscopic colitis risk factors and causes
Doctors don’t know the exact cause of the disease, but several factors are linked to a higher risk:
Medications
- Proton pump inhibitors (like omeprazole for acid reflux)
- NSAIDs (like ibuprofen and naproxen)
- SSRIs (antidepressants like sertraline)
- Statins (for lowering cholesterol)
Autoimmune conditions
- Celiac disease
- Thyroid disorders (especially hypothyroidism)
- Rheumatoid arthritis
In some cases, stopping a triggering medication can help. But for most, it’s a chronic condition that needs long-term care. Current and former smokers are also at higher risk, as well as women due to hormonal changes.
Diagnosing microscopic colitis
The most accurate way to diagnose microscopic colitis is through a colonoscopy with biopsy. A standard colonoscopy may show a normal-looking colon. That’s why tissue samples are essential.
The doctor will take several biopsies from different parts of the colon. These are sent to a pathologist who looks for specific microscopic changes. Without the biopsy, microscopic colitis can easily be missed.
Sometimes, doctors will also often check for:
- Celiac disease with a blood test
- Infections through stool tests
- Thyroid levels with a blood test
Treatment options for GI disorders
Treatment focuses on managing symptoms and reducing inflammation. Most people respond well to medication and lifestyle changes. Dr. Micic says the first-line treatment is usually budesonide, a steroid that works directly in the colon and causes fewer side effects than traditional steroids.
Other medications include:
- Loperamide (Imodium): Helps slow diarrhea
- Diphenoxylate: A stronger anti-diarrheal
- Bile acid binders: Help if bile is causing irritation
- Aminosalicylates or immunosuppressants: Used in rare, severe cases
Diet changes also help. Patients are usually advised to:
- Avoid dairy if lactose intolerant
- Cut out artificial sweeteners like sorbitol or xylitol
- Reduce greasy or high-fat foods
- Drink plenty of fluids with electrolytes to stay hydrated
Although diet doesn’t reduce inflammation, it can reduce symptom flare-ups. Some people may also benefit from working with a registered dietitian.
“Many times, we start off with an oral steroid agent, which has well over 80 to 90% effectiveness early on in the treatment course,” says Dr. Micic. “Unlike systemic steroids, the ones we use are targeted to the colon, so we don’t see the typical side effects like thinning of bones or increased blood pressure.”
Is microscopic colitis chronic?
In most cases, yes. Roughly 80% of patients will have chronic GI symptoms that come and go over time. It’s a lifelong condition, but it can be well managed.
In rare cases, if a specific medication is the cause, symptoms may go away after stopping the drug. But most patients need a combination of medication and lifestyle strategies to stay well.
When to see a gastroenterologist
If you’re having diarrhea that lasts more than two weeks, don’t wait. It could be a sign of something more serious. Microscopic colitis often gets worse over time if not treated.
Also, see a doctor if you have:
- Blood in your stool
- Unexplained weight loss
- Diarrhea after every meal
- Trouble controlling your bowels
These are signs that further testing is needed. A gastroenterologist can help identify the cause and start treatment.
Loyola Medicine’s digestive health care team
Loyola Medicine provides expert care for patients with complex digestive issues. Our gastroenterologists use advanced diagnostic tools and tailor treatments to each patient’s needs.
We also offer virtual digestive health visits, which can be a great first step. During a virtual appointment, you’ll talk with a GI specialist about your symptoms and get advice on what tests or treatments are needed. This is especially helpful if you can’t get in for an in-person visit right away.
Dr. Micic says, “Virtual care is a great way to get started. We can listen to your concerns, recommend next steps, and get you the care you need."
Dejan Micic, MD, is a gastroenterologist at Loyola Medicine, with a special interest in inflammatory bowel disease, including Crohn's disease and ulcerative colitis. Dr. Micic earned his medical degree from the University of Wisconsin School of Medicine and Public Health. He then completed his residency at the University of Michigan Health System.
