Understanding Acoustic Neuromas: Symptoms, Diagnosis, and Treatment
August 1, 2025
Categories: Neurology & Neurosurgery, ENT/Otolaryngology
Tags: acoustic neuroma, vestibular schwannoma, skull base tumor, tinnitus, hearing loss
By John P Leonetti, MD, Otolaryngology and Anand Vasant Germanwala, MD, Neurosurgery


An acoustic neuroma, also known as a vestibular schwannoma, is a noncancerous skull base tumor that develops on the vestibulocochlear nerve which is responsible for hearing and balance. While benign, acoustic neuromas can still cause significant symptoms and complications due to their location near critical structures in the brain. Early detection and individualized treatment planning are essential to preserving quality of life and minimizing long-term effects.
“We don’t rush anyone. Every patient gets an evaluation and then is discussed in our multidisciplinary tumor board, where ENT surgeons, neurosurgeons, radiation oncologists, and other specialists all weigh in. That collaboration ensures multiple providers are looking at a patient from different perspectives and that we are offering the best, most personalized plan of care," says Center Co-Director and Neurosurgeon Anand V. Germanwala, MD.
What causes acoustic neuromas?
Acoustic neuromas (vestibular schwannomas) originate from Schwann cells, which insulate and support nerves. Specifically, these tumors arise on the vestibular portion of the vestibulocochlear nerve which carries balance and hearing signals from the inner ear to the brain.
The exact cause of most acoustic neuromas remains unknown. However, a small percentage of cases are linked to a hereditary disorder called Neurofibromatosis Type II (NF2). This genetic condition leads to the development of multiple tumors on nerves throughout the body, including bilateral acoustic neuromas.
"Acoustic neuromas are benign tumors that originate from the vestibular or balance nerves of the inner ear and as they grow slowly, they destroy the vestibular nerve over several months. This gives the vestibular nerve on the non-tumor side ample time to compensate. Explaining why dizziness is not as common as tinnitus or hearing loss in patients with this type of tumor," says Dr. John P. Leonetti, Co-Director of Loyola Center for Cranial Base Tumors.
When to see a specialist in skull base acoustic neuromas
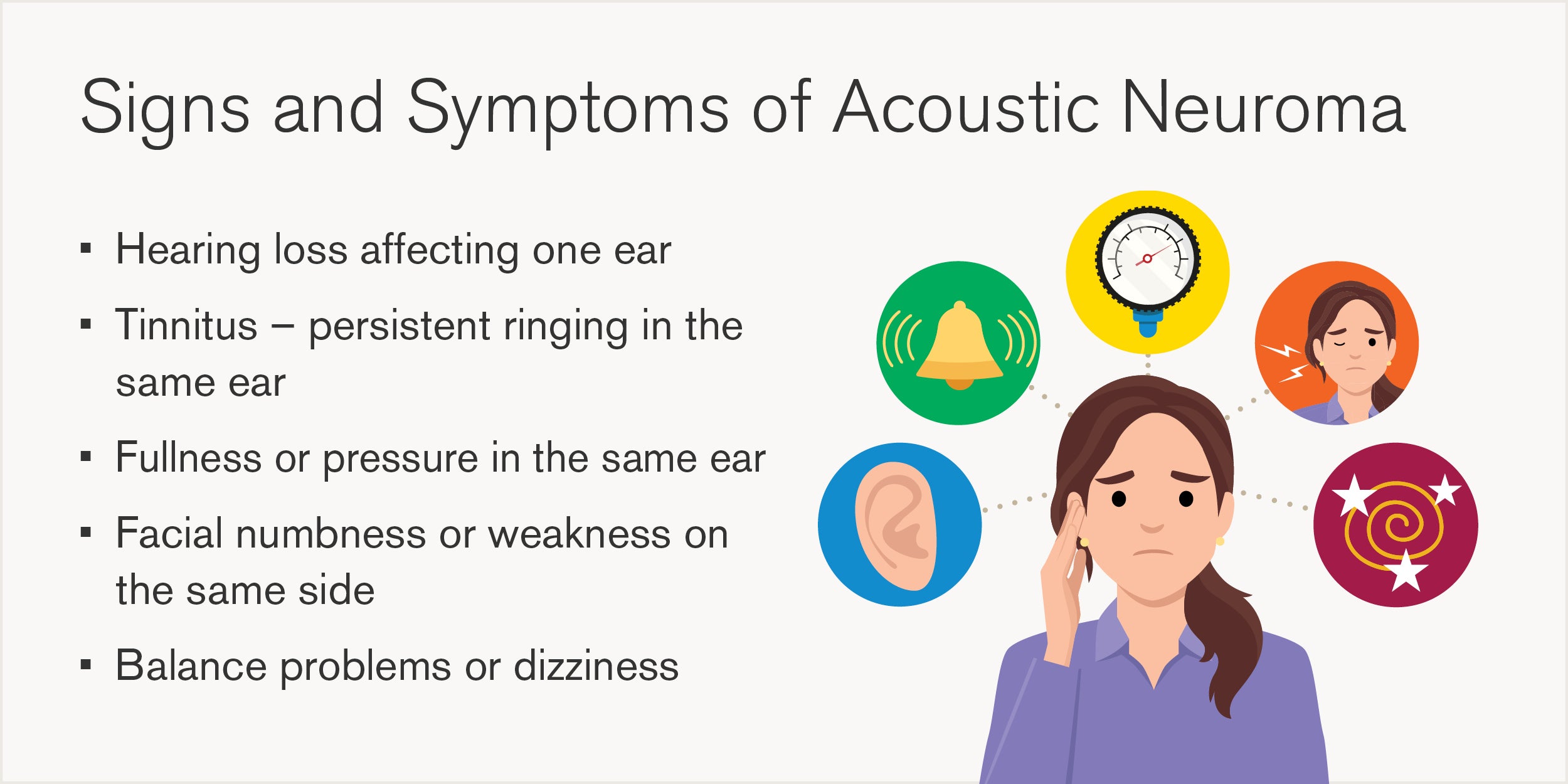
Because acoustic neuromas grow slowly, symptoms often develop gradually and can be easy to dismiss early on. If you experience persistent one-sided hearing loss, tinnitus, ear fullness, facial numbness, and/or unexplained balance problems, it is important to consult a skull base tumor specialist.
Early evaluation allows for more treatment options and a greater likelihood of preserving hearing and nerve function. Loyola’s team includes dedicated otolaryngologists and neurosurgeons who specialize in skull base conditions, ensuring expert care from diagnosis through recovery.
“If a patient is having symptoms and has progressive hearing loss, fullness, and ringing in the ear that doesn’t improve over time, that’s when we start to get concerned," says Dr. Germanwala.
How are acoustic neuromas diagnosed?
The diagnostic process usually begins with a hearing evaluation (audiogram) to assess sound detection across various frequencies. If results suggest an abnormality, especially a pattern indicative of nerve involvement, an MRI with contrast is performed.
This type of imaging allows physicians to clearly visualize the tumor and assess its size, exact location, and relationship to surrounding structures. Currently, an MRI is the gold standard for diagnosing acoustic neuromas and differentiating them from other causes of auditory or vestibular symptoms.
Acoustic neuroma treatment options
Treatment planning at Loyola Medicine is highly individualized and depends on tumor size, location, rate of growth, and the patient’s symptoms and overall health. The main options include:
Observation
For small tumors that are not causing severe symptoms, monitoring with periodic MRIs and hearing tests is often appropriate. Many acoustic neuromas grow slowly, typically 1 to 2 mm per year, and may even remain stable for extended periods. This conservative approach helps avoid unnecessary interventions while keeping a close eye on the tumor’s behavior.
“For many patients with small or stable tumors, the best approach is often observation. We’ll monitor the tumor with MRIs, initially at six months, then annually, to track any growth. Treatments come with risks, so we want to ensure any decision is truly necessary," says Dr. Germanwala.
Stereotactic radiosurgery
This form of highly targeted radiation delivers focused doses to the tumor while sparing surrounding tissues. Known as stereotactic radiosurgery (SRS), it is typically completed in 1 to 5 sessions using advanced robotic systems guided by neurosurgeons and radiation oncologists.
SRS is non-invasive and well-suited for small to medium-sized tumors or for patients who are not good surgical candidates. It is a key part of Loyola’s treatment capabilities and provides excellent control rates with minimal downtime.
Surgical removal
Surgery may be recommended for larger tumors, tumors that are growing, or those causing significant symptoms such as brainstem compression. And sometimes, patients just want the tumor removed. Loyola Medicine offers all acoustic neuroma surgical approaches, including retrosigmoid, translabyrinthine, and middle fossa surgical corridors as well as newer techniques such as potential hearing sparing surgery for smaller tumors, the incorporation of artificial intelligence to guide surgeons, and cochlear implantation to help restore hearing.
However, it's important to stress how seriously Loyola's physicians approach maximally safe resection, a surgical treatment that removes as much of the tumor as possible while preserving surrounding nerves and structures to minimize complications and risks. This approach allows for maximum tumor removal that provides tissue sampling and DNA analysis, which can offer insight into the tumor’s biological behavior and guide follow-up care.
“Surgery for acoustic neuromas is delicate and complex. It requires close collaboration between a neurosurgeon and an ENT surgeon who specialize in skull base tumors. At Loyola, we have the experience and capability to offer all surgical approaches with very experienced teams, and we tailor each recommendation to the patient’s unique case," says Dr. Germanwala.
No Treatment
In rare cases, a patient may choose not to undergo any intervention at all. While not typically advised, Loyola’s team respects patient autonomy and ensures that each decision is fully informed and supported.
Living with an acoustic neuroma
While acoustic neuromas are benign, they can still affect quality of life. Long-term outcomes depend on the tumor’s size, location, and the chosen treatment path. Some patients may have persistent or even complete hearing loss, balance issues, facial numbness, or facial weakness. Loyola Medicine offers robust support services to address these challenges, including:
- Audiology services and hearing aids
- Vestibular rehabilitation for balance
- Facial nerve therapy
- Counseling and patient education
- Cochlear implants
The team is also engaged in ongoing research, including the use of artificial intelligence to predict surgical outcomes and preserve hearing whenever possible.
Recovery and follow-up care
Surgical recovery varies depending on the tumor’s size and complexity of the procedure. Most patients stay in the hospital for about three days: one night in the ICU and two nights on the general floor. Full recovery typically takes four to six weeks, during which time patients are encouraged to rest, walk, and attend follow-up appointments.
Radiation patients typically return to normal activities the following day, with only mild side effects such as headache or localized pressure.
Loyola provides structured follow-up care, including:
- Postoperative MRIs to assess tumor removal
- Ongoing annual imaging to monitor for recurrence
- Audiology visits to track hearing
- Multidisciplinary tumor board evaluations for complex cases
Why Loyola Medicine for acoustic neuroma care?
When it comes to the diagnosis and treatment of acoustic neuromas, Loyola Medicine stands as a recognized leader in the Chicagoland region. Over the last 25 years, our expert teams have performed more than 1,500 acoustic neuroma surgeries, making Loyola one of the busiest and most experienced acoustic neuroma and comprehensive skull base centers in the country. This high volume directly translates to better outcomes, fewer complications, and more personalized care for our patients.
Our program is anchored by the Center for Cranial Base Surgery, a multidisciplinary hub that brings together fellowship-trained neurosurgeons, otolaryngologists, radiation oncologists, and audiology specialists. This collaborative approach ensures that each patient receives a tailored treatment plan—whether that involves observation, radiation, surgery, or a combination of therapies.
Designated as a Skull Base Center of Excellence by the North American Skull Base Society, Loyola’s program is also at the forefront of clinical research and innovation, including advanced imaging techniques and AI-guided surgical planning. From diagnosis to long-term follow-up, our team is committed to delivering the highest standard of care with compassion, precision, and expertise.
“What sets Loyola apart is our unmatched experience and truly collaborative approach. As the first center of its kind in the Midwest, we’ve treated over 5,000 patients with tumors above the clavicle, regardless of type. Our outcomes speak for themselves, including shorter hospital stays, fewer complications, and a team that leads not just in care, but in research,” says Dr. Leonetti.
Ready to take the next step?
To schedule an appointment at the Center for Cranial Base Tumors, please complete the appointment request form by clicking below. A team member will follow up with you for the next steps. Let us help you move forward with confidence and hope.
John Leonetti, MD, is a leading otolaryngologist at Loyola Medicine specializing in otology and skull base surgery. As Program Director of the Loyola Center for Cranial Base Surgery, he brings decades of experience in treating complex tumors and restoring facial nerve function, particularly in patients with Bell’s palsy. A pioneer in his field, Dr. Leonetti has performed thousands of procedures and remains at the forefront of clinical care and academic research.
Anand V. Germanwala, MD is Co-director of the Loyola Center for Cranial Base Surgery, Professor of Neurological Surgery and Otolaryngology, and the Interim Chair and Residency Program Director for the Department of Neurological Surgery at Loyola University Chicago Stritch School of Medicine. Having trained at the University of Pittsburgh Medical Center and received advanced fellowship training in cranial base surgery at Johns Hopkins University, he specializes in skull base and brain tumor surgery.
