Take Control of Your Digestive Health: A Guide to Understanding and Managing Diverticulitis
June 23, 2025
Categories: Digestive Health
Tags: diverticulitis
By Amanda Blanche Siegel, MD | Loyola Medicine, Digestive Health
If you’ve been diagnosed with diverticulitis, you’re not alone and you’re not without options. This common digestive condition affects millions of adults, especially those over 40. While it can be painful and disruptive, it’s also highly manageable with the right care and information.
Whether you’re navigating your first flare-up or supporting someone who has, this blog will help you understand what diverticulitis is, how it’s treated, and what you can do to prevent future episodes.
What is diverticulitis?
Diverticulitis is the inflammation or infection of small pouches, called diverticula, that form in the wall of the colon. These pouches are common, especially as we age, and are usually harmless (a condition known as diverticulosis). But when one or more become inflamed, it leads to diverticulitis.
“Diverticuli are the small outpouchings that are present in the colon,” explains Amanda Siegel, MD, a gastroenterologist at Loyola Medicine. “They develop at areas in which there's weakness in the muscle that go around the colon.”
While the exact cause of inflammation isn’t fully understood, one theory is that stool or food particles can get trapped in these pouches, triggering an immune response. “We hypothesize that bits of stool or food residue can get stuck in those pouches, and that can create an inflammatory response,” Dr. Siegel adds.
Common diverticulitis symptoms to watch for
The most recognizable symptom of diverticulitis is persistent pain in the lower abdomen, usually on the left side. Other symptoms may include:
- Fever
- Constipation (more common) or diarrhea
- Nausea or vomiting
- Bloating or tenderness
- Loss of appetite
“It’s pain that doesn’t subside and that comes on fairly quickly,” Dr. Siegel says. Diverticulitis symptoms can vary in intensity. Some people may experience mild discomfort, while others may have severe pain that interferes with daily activities. If you’re experiencing these symptoms, especially with a fever or digestive changes, it’s important to contact your health care provider.
How is diverticulitis diagnosed?
Diagnosis typically begins with a physical exam and a review of your symptoms. However, the most definitive tool is a CT scan, which can detect inflammation and rule out complications like abscesses or perforations.
“The CT scan will look for areas with active inflammation in the colon associated with one of those little outpouchings,” says Dr. Siegel. “If a patient were to call me with symptoms concerning for diverticulitis, I would order a CT scan to be performed that day.”
Early diagnosis is key to preventing complications and determining the best course of treatment.
When to seek emergency care for gastrointestinal symptoms
While many gastrointestinal problems can be managed at home, some symptoms require urgent medical attention. Go to the emergency room if you experience:
- Severe or worsening abdominal pain
- High fever
- Inability to eat or drink
- If you’re an older adult or someone with a weakened immune system with symptoms
“Severe lower abdominal pain, high fever, inability to tolerate food or liquids; those would be situations where we might send patients to the emergency room,” Dr. Siegel advises.
Prompt care in these situations can prevent more serious outcomes, such as bowel perforation (a hole in the intestinal wall) or widespread infection.
Treatment for diverticulitis: What to expect
Most cases of diverticulitis are treated with oral antibiotics and rest. Symptoms typically improve within 10 to 14 days.
During recovery, patients are often advised to follow a low-fiber or liquid diet for a few days to allow the colon to rest. As symptoms improve, fiber is gradually reintroduced.
"A small percentage of patients require IV antibiotics and hospitalization," Dr Siegel notes. Rarely, complications like abscesses or perforations require surgical intervention.
Long-term outlook and recurrence of GI issues
After recovery, your doctor may recommend a follow-up colonoscopy, usually about eight weeks later, to rule out other conditions like colon cancer.
If you experience recurrent episodes of diverticulitis, your doctor may refer you to a surgeon to discuss removing the affected portion of the colon. This is typically considered after two or more episodes in the same area.
Diet and lifestyle modifications to avoid flare-ups
There’s a lot of confusion about what to eat after a diverticulitis diagnosis. For years, patients were told to avoid nuts, seeds, and popcorn. But that advice may be outdated.
“More recent studies have shown that there is no clear association between eating nuts and seeds and diverticulitis,” says Dr. Siegel.
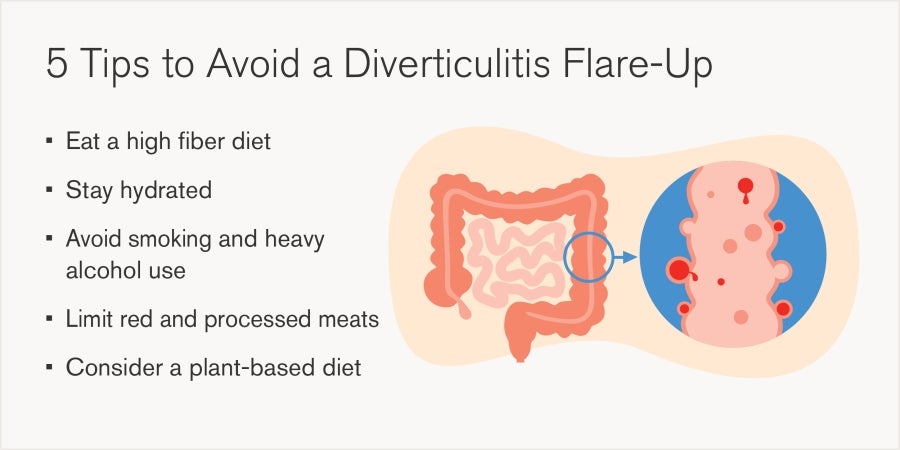
These changes not only support colon health but also benefit your overall well-being.
Reassurance for patients with digestive health concerns
A diverticulitis diagnosis can feel overwhelming, but the prognosis is generally excellent. “Most patients are expected to make a complete recovery without any major complications,” says Dr. Siegel. “This is typically a treatable condition.”
With the right treatment, lifestyle changes, and follow-up care, you can take control of your digestive health and reduce the risk of future flare-ups.
Amanda Blanche Siegel, MD, is a board-certified gastroenterologist with Loyola Medicine, specializing in the diagnosis and treatment of digestive disorders. She is also board-certified in internal medicine. Dr. Siegel earned her medical degree from Northwestern University Feinberg School of Medicine, where she also completed her residency and fellowship training. Her clinical interests include irritable bowel syndrome, celiac disease, GERD, chronic diarrhea, constipation, and abdominal pain.
