If you’ve been struggling with chronic nasal congestion, frequent sinus infections, or difficulty breathing through your nose, you might be surprised to learn that a deviated septum could be the root cause. While many people live with this condition unknowingly, its impact on sinus and respiratory health can be significant.
What is a deviated septum?
The nasal septum is the wall of cartilage and bone that divides your nasal cavity into two sides. Ideally, it sits in the center, allowing equal airflow through both nostrils. A deviated septum occurs when this wall is off-center, making one nasal passage smaller than the other. Most people have some degree of deviation, but not all cases are clinically significant.
“It’s a generic term that just means the septum isn’t perfectly midline,” says Chirag Patel, MD, an Ear, Nose and Throat (ENT) specialist at Loyola Medicine. “The majority of people have some deviation, but whether it’s relevant depends on how it affects their breathing.”
How a deviated septum causes sinus problems and difficulty breathing
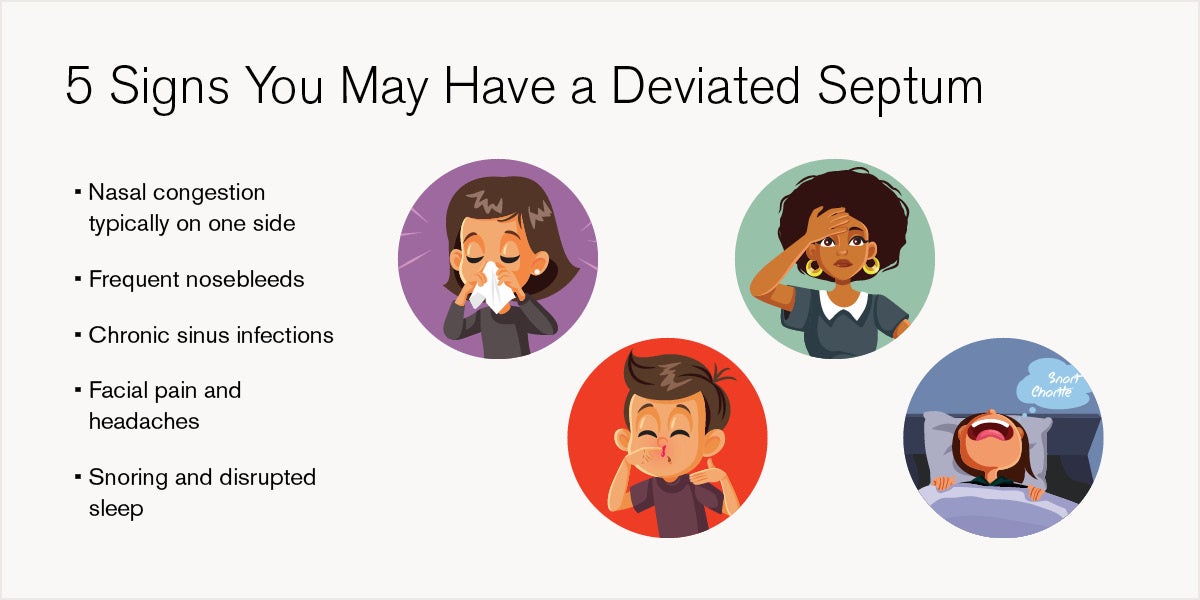
A deviated septum can lead to a range of respiratory symptoms, especially when it obstructs airflow. These can include:
- Nasal obstruction: Difficulty breathing through one or both nostrils, often worse when lying down.
- Snoring and sleep disruption: Blocked airflow can contribute to snoring or even sleep apnea.
- Chronic sinus infections: Impaired drainage can lead to recurring infections, facial pain, and headaches.
- Nosebleeds: Dryness and irritation from uneven airflow can increase the risk.
- Reduced oxygen intake: Some patients report fatigue or lightheadedness due to poor airflow.
A deviated septum can also exacerbate other conditions like allergies or enlarged turbinates, compounding congestion and discomfort. Thankfully, most cases are developmental, meaning the septum grew off-center during childhood. While injury can worsen the condition, it generally remains stable in adulthood.
However, if breathing worsens over time, it may signal another issue, such as nasal polyps, chronic sinusitis, or even tumors.
“If your breathing is getting worse, that suggests something more serious,” says Dr. Patel. “And that’s something that should always be assessed.”
Diagnosing a deviated septum
Diagnosis begins with a thorough patient history and physical examination. ENT specialists will assess symptoms like which side feels more congested, whether symptoms are constant or intermittent, and any history of trauma or sinus infections.
During the exam, doctors look inside the nose for structural issues, polyps, infection, or tumors. They also evaluate the external nasal structure, as soft cartilage or narrow nostrils can contribute to breathing problems.
“If I see a septum deviated to the left and the patient says their left side doesn’t move enough air, that’s a strong correlation,” says Dr. Patel.
Non-surgical treatment options for deviated septum
While a deviated septum is a structural issue, non-surgical treatments can help manage symptoms, especially when nasal inflammation or other factors are involved. These can include:
- Nasal corticosteroids: Reduce inflammation and improve airflow
- Decongestants: Temporarily shrink swollen nasal tissues
- Antihistamines: Help with allergy-related symptoms
- Nasal strips or dilators: Mechanically widen the nostrils to improve airflow
- Nasal irrigation: Saline rinses help clear mucus and allergens
- Breathing exercises and yoga: May enhance respiratory function
These treatments don’t correct the deviation but can offer meaningful relief, especially for mild cases or temporary congestion.
What is septoplasty and when is it needed?
If symptoms persist despite conservative treatment, septoplasty, a surgical procedure for a displaced nasal septum, may be recommended. This outpatient procedure involves straightening the septum by removing or repositioning bone and cartilage. However, this approach depends on the location of the deviation.
- Posterior deviations (further back in the nose): Typically corrected through a small internal incision.
- Anterior deviations (near the front): May require a more complex procedure called functional rhinoplasty, which involves reshaping and reinforcing the nasal structure.
Recovery from septoplasty is usually quick. Most patients return home the same day and resume normal activities within a week or two.
You don’t have to live with chronic congestion
A deviated septum is common, but that doesn’t mean you have to suffer. If you’re experiencing persistent nasal blockage, sinus infections, or sleep disturbances, it’s time to seek expert care.
At Loyola Medicine, ENT specialists offer comprehensive evaluations and personalized treatment plans, whether that means medication, lifestyle adjustments, or minimally-invasive surgery.